- Journal List
- Am J Public Health
- v.102(5); May 2012
- PMC3325336

Implicit Stereotyping and Medical Decisions: Unconscious Stereotype Activation in Practitioners' Thoughts About African Americans
 Corresponding author.
Corresponding author.G. B. Moskowitz and J. Stone originated the research topic. G. B. Moskowitz designed the study and led the writing of the article. A. Childs developed the research materials and collected and coded the data. G. B. Moskowitz and A. Childs conducted the statistical analyses. J. Stone helped revise the article.
Abstract
Objectives. We investigated whether stereotypes unconsciously influence the thinking and behavior of physicians, as they have been shown to do in other professional settings, such as among law enforcement personnel and teachers.
Methods. We conducted 2 studies to examine whether stereotypes are implicitly activated in physicians. Study 1 assessed what diseases and treatments doctors associate with African Americans. Study 2 presented these (and control terms) to doctors as part of a computerized task. Subliminal images of African American and White men appeared prior to each word, and reaction times to words were recorded.
Results. When primed with an African American face, doctors reacted more quickly for stereotypical diseases, indicating an implicit association of certain diseases with African Americans. These comprised not only diseases African Americans are genetically predisposed to, but also conditions and social behaviors with no biological association (e.g., obesity, drug abuse).
Conclusions. We found implicit stereotyping among physicians; faces they never consciously saw altered performance. This suggests that diagnoses and treatment of African American patients may be biased, even in the absence of the practitioner's intent or awareness.
Health care professionals learn that some diseases may be associated with various population groups. Doctors and nurses, for example, need to know if some categories of people are more likely than others to manifest specific symptoms and diseases. Ashkenazi Jews have a higher prevalence of Tay-Sachs disease than other groups. Hypertension is more prevalent among African Americans and Native Americans than White Americans. Such facts are essential to medical training and depict an accurate stereotype of these social groups. (Stereotype is defined as the knowledge we possess about, and associate with, a particular human social group.1) Thus, health care workers are taught to categorize individuals according to social groups so that patients may be accurately stereotyped along health-relevant domains.
Research in psychology has revealed that stereotypes, when factual, are an aid to information processing and facilitate accurate judgment and smooth social interaction.2 However, such research has also revealed that, unbeknownst to the perceiver, when the stereotype is invoked it also typically triggers inaccurate beliefs about the social group that ascribe predominantly negative qualities to the group and its members.3 For many social groups, the negative components of the stereotype are the more dominant association to the group, causing a person's overall reaction to a member of the group to be infused—unintentionally—with negative qualities. This is not the only unintended effect of categorizing people into social groups. These triggered negative components of the stereotype (which if they rose to conscious thought would be denounced and rejected) exert a well-established influence on perception, judgment, evaluation, and behavior.4,5 The effect is a dissociation between a person's conscious experience of being unbiased and a person's actual response, which is often guided by unconscious negative stereotypes. The influence of such unconsciously triggered negative and inaccurate components of a stereotype has been shown to bias judges’ sentencing decisions,6 employers' hiring decisions,7 teachers' evaluations of students,8 police officers' decisions to respond with shows of force,9,10 and people's judgments about one another's personality during everyday encounters.11
Like all other members of society, medical professionals know the social stereotypes of groups and thus are presumably subject to having stereotypes similarly unconsciously triggered. These implicit stereotypes could affect their diagnoses, treatment recommendations, expectations about whether a patient will follow a prescribed treatment, and both verbal and nonverbal behavior toward patients during professional interactions, despite their intention to avoid such biases in conduct. We therefore sought to illustrate that all aspects of stereotypes, not just the factually correct information, are triggered in the minds of medical doctors without their awareness.
A second unintended effect of categorizing a person as a group member is that the correct aspects of the stereotype can influence people at an undesired moment and lead to exaggerated and inaccurate judgments. It has been shown, for example, that expectations about a person unknowingly affect how a relevant behavior is identified: if we expect a person to be sad, we not only identify their tears as tears of sadness (as opposed to joy), but also infer an extreme amount of sadness (more than if no expectation had existed).12 We consciously experience our inference that the person is sad, but do not realize (1) the role our expectations play in producing that experience, (2) the role expectations play in delivering an inaccurate assessment of the degree to which the person is sad, and (3) the possibility that the expectation has led us to the wrong conclusion because the person may be shedding tears for another reason, such as joy or pain. Medical professionals are armed with such expectations by their accurate (and inaccurate) stereotypes, and thus, if stereotypes are activated, doctors can be led astray regarding both the severity of a patient's symptoms and the diagnosis—even if the stereotypical information they are using is perfectly correct. This is another reason we sought to establish whether medical doctors unknowingly allow stereotypes to guide their professional conduct.
Finally, categorizing people into groups leads to a host of affective or attitudinal consequences of which people may be unaware. We tend to dislike people from groups that are different from our own once we have brought group membership into play as a relevant domain with which to define a person, even when no real history of intergroup conflict or rational basis for such dislike exists.13,14 We also evaluate people from groups immediately and unknowingly, triggering what are referred to as implicit attitudes.15 Although explicit attitudes influence consciously controlled action, implicit attitudes guide nonverbal responses and other behaviors that are more difficult to control.16 For example, in an experiment by Green et al., physicians read the same vignette of a 50-year-old man with chest pain accompanied by an electrocardiogram suggesting he had anterior myocardial infarction.17 Half the physicians were shown a picture of a White patient, and the other half saw a picture of an African American man. The researchers found that implicit attitudes negatively influenced diagnosis and treatment recommendations (explicitly stated attitudes did not).
The psychological literature explains this implicit form of bias with a model of stereotyping5,11,18 that reveals it to unfold across a series of mental processes, or stages:
a person is identified and categorized as a group member (this can occur either consciously or unconsciously);
this is typically followed within 300 milliseconds by the unconscious act of retrieval from memory of the most dominant associations to the group (often the negative and positive elements of a group stereotype);
this stereotype is held in working memory outside of conscious awareness, attaining what is called a state of accessibility, and therefore more likely than other potential information to be used in directing subsequent cognitive, affective, and behavioral responses;
conscious responding is initiated and is moored to the unconscious stereotypes that were triggered, resulting in an undetected bias in how a person is perceived, evaluated, diagnosed, and treated; and
people may attempt to control the impact of the stereotype on their responses; the most common form of control is attempts to compensate or correct for the bias if it is detected (although control can occur even if bias is undetected2,3).
Our research focused on illustrating that stereotype accessibility occurs during the first 3 of these stages in a sample of medical doctors. The resulting mental state is a distinct phase of cognition that is dissociable from subsequent stages of cognition in which the accessible stereotype is used to shape an individual's response.5,18,19 A medical professional may remain naive to both a stereotype's accessibility and its use, but its accessibility is the more primary psychological event and must occur for a stereotype to bias reactions to a person. We focused on 2 questions relating to the accessibility of health care professionals’ stereotypes: (1) Are stereotypes made accessible without awareness whenever one person categorizes another as a member of a stereotyped group? (2) Does this unconscious event result in both the factual information associated with a group and the incorrect, undesired elements of the stereotype (which are explicitly rejected) attaining accessibility and heightened potential influence? We carried out 2 studies to answer these questions.
In recent years several empirical investigations have been conducted of how unconscious attitudes affect medical professionals.17,20 However, no study has examined whether doctors have stereotypes unconsciously triggered or the role that implicit stereotype activation has on diagnosis or treatment. We hypothesized that in addition to implicit attitudes (general emotional reactions), implicit stereotypes (specific knowledge about the group) are an underlying causal force that guides the differential reactions to minority and majority group members that were documented by the 2009 National Healthcare Disparities Report from the US Department of Health and Human Services.21 Although a small literature has accumulated that reveals that doctors' unconscious attitudes are triggered when encountering minority group members, these studies do not show that they also have stereotypes triggered. Such a finding would be foundational for linking the mental processes detailed in the multistage psychological model of stereotyping to health disparities.
METHODS
We used the following methods to assess the conscious and unconscious stereotypes of African Americans and to examine if such stereotypes are triggered outside of awareness.
Study 1
To examine what diseases and disorders might be implicitly associated with African Americans as part of a stereotype, we first determined what diseases and disorders are explicitly associated with African Americans. We surveyed physicians to discover what they believed the cultural stereotypical diseases associated with African Americans were in the medical community at large (not their personal beliefs, but shared stereotypes).
We asked 3 physicians at 3 hospitals located in different regions of the United States to relay our request for participation (by filling out a Web-based survey) to colleagues at their institutions. Sixteen licensed doctors responded to this request and participated by logging in to our Web page and completing the anonymous survey.
We created an online survey with SurveyMonkey (Palo Alto, CA). Participants first saw this introduction:
The purpose of this study is to understand your awareness of diseases stereotypically associated with African Americans in the medical community. You do not need to endorse or believe stereotypes in order to know what they are and that they exist in your profession. We are interested in your knowledge of specific stereotypes, your ability to report what the medical community in general thinks, not what you personally think.
They then listed any diseases doctors in America associate with African Americans more than other groups. We retrieved results on an Excel spreadsheet (Microsoft Corp, Redmond, WA) downloaded from SurveyMonkey.
Study 2
We hypothesized that when a person thinks about another in terms of a group, even when merely seeing a group member in peripheral vision, thoughts of the stereotype of that group are unconsciously triggered as a natural consequence of the group having been identified (categorization leads to stereotype activation). Perhaps the best test of whether this process is unconscious relies on 2 distinct methodological tools. The first is to trigger the stereotype without the person being tested having any conscious recognition of even seeing a member of the group in question and therefore being unaware that categorization or stereotype activation has occurred. The second is to assess whether the stereotype has been activated without the person being tested realizing that stereotyping is the subject of study.
To accomplish these methodological goals, we employed procedures commonly used in psychological research.22 We triggered the stereotype by presenting our research participants with faces of members of a stereotyped group (African American men) at speeds so fast that they never consciously detected having seen any image at all. That is, we relied on subliminal exposure of the individual to the face. We assessed stereotype activation or accessibility with a reaction time procedure in which participants responded to items on a screen as quickly as possible. The logic of such procedures is that if a participant recently thought about an item, consciously or not, reaction times on exposure to that item would be faster because it had been retrieved from long-term memory.23–25 If physicians hold an implicit association between specific diseases and African Americans, then there should be a difference in how quickly they can identify or categorize those medical terms (versus medical terms not part of the stereotype) as a function of what type of face was subliminally presented. A priming effect26 should emerge in which response times to stereotype-relevant items would decrease if the responder is subliminally primed with an African American man's face. No such facilitation in response times to these stereotypical diseases should occur after seeing White faces or to nonstereotypical diseases that follow African American faces. This pattern would indicate that the stereotype was unconsciously triggered upon unconsciously detecting the face.
Eleven White doctors, 3 women and 8 men, from 3 hospitals (different from those used in study 1), in New York, New Jersey, and Pennsylvania volunteered to participate. Participants completed the experiment individually on a computer. Instructions were presented on the computer, and the participants were asked to hit any key when they understood the instructions to continue to the task.
Reaction time task.
Participants were asked to identify whether words that were to appear on the screen were names of diseases or treatments, or not, by pressing buttons marked yes or no on the keyboard. They were asked to respond as quickly and accurately as possible, and were given no more than 1.5 seconds for each response. They were informed the task would involve many trials, and that each trial would begin with a marker to indicate that a word was about to appear, directing their gaze and readying attention for the response, as well as clearing the previous response from their mind. The task began with 16 practice trials, followed by 168 trials.
Each trial began with the marker appearing in the center of the screen for 250 milliseconds. This marker appeared in the same location each time, and was immediately followed by an identically sized image of a man's face appearing for 10 milliseconds. This image was then replaced with the initial marker for another 125 milliseconds, thus giving the appearance to participants of a 385-millisecond-long uninterrupted picture of a marker. The face that appeared subliminally within this marker belonged to either an African American or a White man. We used photographs (each 150 × 200 pixels) of African American men and White men that were part of previous research.27,28 Immediately after seeing the marker, participants saw a word randomly selected from a pool of 84 words. Each word appeared in 2 separate trials, once subliminally primed with an African American man's face and once with a White man's face.
Word stimuli.
Stimuli consisted of medical terms, nonmedical terms, and nonwords. Our interest was in the medical terms, which were either diseases revealed by study 1 to be stereotyped as African American (drug abuse, HIV, hypertension, obesity, sarcoidosis, sickle cell anemia, stroke), or medical terms that were not mentioned by participants in study 1 and thus not thought to be associated with African Americans (chicken pox, Crohn's disease, leukemia, Lyme disease, meningitis, multiple sclerosis, pneumonia, scoliosis). We added renal cell cancer to the list of stereotypical diseases presented because it had been used in this way in past research.29 We also divided diseases into 2 types: with or without a known genetic component. The former group comprised hypertension, sickle cell anemia, stroke, sarcoidosis, renal cell cancer, Crohn's disease, leukemia, multiple sclerosis, and scoliosis. HIV, drug abuse, obesity, Lyme disease, meningitis, pneumonia, and chicken pox were classified as having no genetic link.
Analyses.
The experiment had a 2 × 2 × 2 × 2 mixed-factorial design. The within-participant variables were prime type (African American face versus White face), disease type (stereotype versus nonstereotype), and genetic predisposition (yes versus no). The between-participant variable was a counterbalancing factor of whether the Z or the forward slash key was associated with a yes or no response.
We performed a 2 × 2 × 2 × 2 within-subject analysis of variance with participants’ reaction time to words as the dependent variable, and prime type, disease type, counterbalancing factor and genetic predisposition as the independent variables. To further examine the predicted prime-type-by-disease-type interaction, we performed t tests on the means for stereotypical diseases and nonstereotypical diseases following African American faces or White faces.
RESULTS
In study 1, all respondents identified themselves as licensed medical doctors working in the United States. We determined which diseases were most frequently listed and therefore represented stereotypical African American conditions. Participants named a total of 36 diseases. Hypertension was most often mentioned, with 15 of the 16 doctors listing it as a stereotypical disease. Sickle cell anemia was the second-most-reported disease, with a frequency of 12, followed by stroke (reported by 11 of the 16 doctors). HIV and coronary artery disease were each identified 8 times, and drug abuse, obesity, and sarcoidosis 6 times.
In study 2, no participants expressed suspicion about the nature of the experiment or reported having seen any faces. The counterbalancing factor (computer key) revealed no reliable effect, so we excluded it from further analysis.
Two reliable effects emerged from our analysis of variance. A main effect for genetic predisposition revealed simply that response times to diseases that had a genetic predisposition (mean = 779 ms) were slower than to diseases with an environmental origin (mean = 730 ms; F(1,10) = 10.46; P
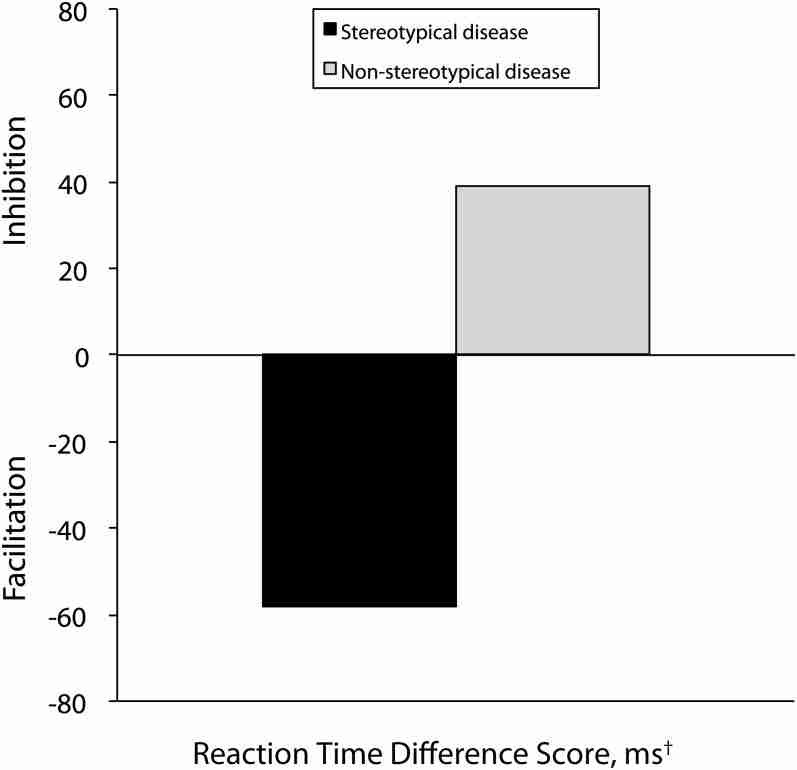
The predicted prime-type-by-disease-type interaction was reliable (F(1,10) = 9.98; P t(10) = 2.33; P t(10) = −3.23; P
As expected, we detected no reliable difference in reaction times to stereotypical versus nonstereotypical diseases that followed White faces. Nor was there an effect of disease origin, genetic or behavioral. Figure 1 shows responses to stereotypical and nonstereotypical diseases expressed as a difference score between reaction times to a word following an African American face minus the reaction time to the same words following a White face. Facilitation is reflected by a negative number (faster response to words following an African American face).
DISCUSSION
Across 2 experiments we identified stereotypes of African Americans that are held in the medical community and the ease with which those stereotypes can be triggered in individual members of that community. This triggering occurs without awareness, as illustrated here, by one never having been aware of having seen a face (subliminal presentation).
Study 1
In study 1, we identified diseases that physicians believed the medical community explicitly associates with African Americans and separated these into 2 groups: conditions that are believed to have a genetic component that predisposes an individual from a specific group to disease (hypertension, stroke, sickle cell anemia, coronary artery disease, sarcoidosis) and those with environmental or behavioral origins (obesity, HIV, drug abuse).
This distinction relates to stereotype accuracy. If African Americans have a genetic predisposition to a disease, then a stereotype that includes this disease is accurate—and hence potentially efficient to use. However, if behavior can cause the condition in anyone, only an established statistical association with African Americans would justify the assumption. For example, many African Americans are known to have a genetic predisposition to sickle cell anemia, but stereotypes about the prevalence of drug abuse among African Americans are not similarly supported by evidence. Data from a 2007 report of the Substance Abuse and Mental Health Services Administration30 reveal that African Americans are less likely than Whites to have injected heroin, cocaine, stimulants, or methamphetamine. A 2003 report shows no statistical differences between these groups in overall illicit drug use (Whites 8.3%, African Americans 8.7%).31 Therefore a doctor's association of African Americans with drug abuse would be inaccurate and unwarranted. It is possible that physicians associate both accurate and inaccurate stereotypical beliefs with various social groups because of cultural messages they have acquired in addition to the medical knowledge imparted in their training.
Study 2
In study 2, we found that physicians responded faster to terms for conditions with environmental origins. This could be attributable to participants being less familiar with diseases with genetic causes or to their slightly longer or harder-to-read names. Our more important results concerned the effects of subliminal faces on physician responses. Our participants implicitly associated specific diseases with African Americans. This is important because (1) it occurred without the doctors realizing they were invoking stereotypes (or even that they were thinking about African Americans), suggesting that stereotypes influenced them in ways and at times they did not consciously intend, and (2) these implicit associations were apparent for both conditions associated with lifestyle choices and diseases associated with genetic predisposition. Implicit stereotypical beliefs about African Americans may be accurate and medically justifiable, and they may equally have no basis in medical evidence.
Our aim was to examine whether implicit stereotyping exists among medical doctors, because it may bias diagnoses of and treatment recommended to African American patients, even in the absence of intent or awareness by the practitioner. Because the triggering of the stereotype and its subsequent influence are 2 dissociable steps, we focused, in this initial study, on whether stereotypes are automatically associated with social groups. Subsequent research must examine how these unconsciously triggered beliefs influence responses. If diseases such as sarcoidosis and drug abuse spring to a doctor's mind more quickly when examining an African American patient, they may crowd out other possible diagnoses even in the presence of symptoms that are consistent with a variety of diseases.
Hundreds of experiments on the psychology of priming effects in nonmedical fields have established this phenomenon. In many cases, an accurate stereotype may be useful. But in many other situations, even if the stereotype is accurate, the individual's symptoms may not be best explained by the stereotypical diagnosis. Another danger is that symptoms may be perfectly aligned with the stereotypical diagnosis, but implicit assumptions may lead to an exaggerated sense of the severity of the symptoms. Most seriously, a stereotype may not be accurate, and a particular disease may not actually be statistically associated with the group the doctor (because of stereotypes learned from the community) has in mind, leading to biased responding.
Conclusions
We recognize that health disparities arise from a complex set of factors: genetic and biological antecedents, socioeconomic predictors, and psychological processes that affect the dynamic between patients and health care professionals. We hypothesize that implicit stereotyping is an important element in the psychology of physician decision-making. Implicit stereotyping among health care providers presents 2 dangers: (1) inaccurate components of a stereotype may be used in diagnosis and treatment without conscious knowledge of this influence, (2) even an accurate stereotype may unduly influence diagnosis and treatment.
Stereotypes develop because they help make us more efficient processors of information, able to focus on greater amounts of information and to do so more quickly.32 Sometimes, however, efficiency is the enemy of accuracy, and in a medical context, the consequences of an inaccurate or incomplete diagnosis could be severe. It is therefore important to understand the unconscious nature of stereotype activation. Although doctors often use stereotypes and are fully aware of the positive consequences of such conscious thoughts, they may also be activating unintended consequences associated with unconscious stereotyping that seemingly occurs every time they have any thought of a patient's social group. We found that stereotypes were triggered by subliminal cues that doctors could not possibly be aware of.
These findings have implications for cultural competency training programs. Recently, findings that implicit bias may be exacerbated by attempts to warn people of explicit bias has led to calls to redesign such programs.33,34 This has been a concern of the legal community, police academies, and medical and nursing schools.34 Our ultimate goal is to find effective ways to teach competency to medical professionals so that both explicit and implicit bias will be reduced, along with the undesirable effects of stereotypes. Such training will allow medical professionals to attain their goal: to help and serve all people through the unbiased provision of health care.
Acknowledgments
This study received funding from the Lehigh University College of Arts and Sciences Dean's New Directions Fellowship. It was also supported by the National Center on Minority Health and Health Disparities (grant R01MD005902).
Note. This article is solely the responsibility of the authors and does not necessarily represent the official views of the National Center on Minority Health and Health Disparities or the National Institutes of Health.
Human Participant Protection
The Lehigh University institutional review board approved the research. Participants gave informed consent.
References
Articles from American Journal of Public Health are provided here courtesy of American Public Health Association