Considerations for Wearing Masks
Help Slow the Spread of COVID-19
- CDC recommends that people wear masks in public settings and when around people who don’t live in your household, especially when other social distancing measures are difficult to maintain.
- Masks may help prevent people who have COVID-19 from spreading the virus to others.
- Masks are most likely to reduce the spread of COVID-19 when they are widely used by people in public settings.
- Masks should NOT be worn by children under the age of 2 or anyone who has trouble breathing, is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.
- Masks with exhalation valves or vents should NOT be worn to help prevent the person wearing the mask from spreading COVID-19 to others (source control).
Evidence for Effectiveness of Masks
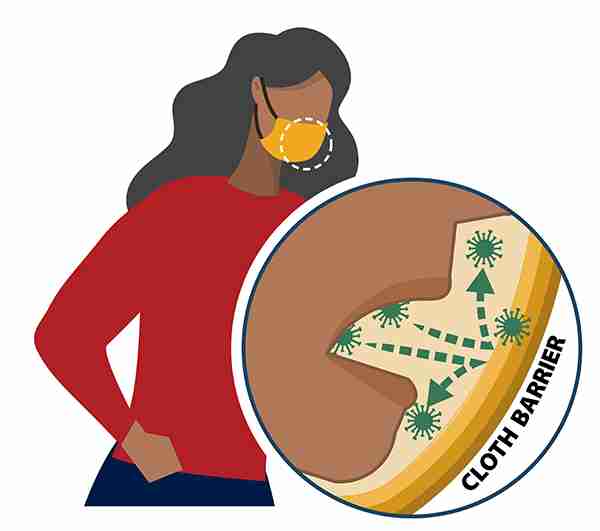
Masks are recommended as a simple barrier to help prevent respiratory droplets from traveling into the air and onto other people when the person wearing the mask coughs, sneezes, talks, or raises their voice. This is called source control. This recommendation is based on what we know about the role respiratory droplets play in the spread of the virus that causes COVID-19, paired with emerging evidence from clinical and laboratory studies that shows masks reduce the spray of droplets when worn over the nose and mouth. COVID-19 spreads mainly among people who are in close contact with one another (within about 6 feet), so the use of masks is particularly important in settings where people are close to each other or where social distancing is difficult to maintain. CDC’s recommendations for masks will be updated as new scientific evidence becomes available.
Who Should Wear A Mask?
General public
- CDC recommends all people 2 years of age and older wear a mask in public settings and when around people who don’t live in your household, especially when other social distancing measures are difficult to maintain.
- COVID-19 can be spread by people who do not have symptoms and do not know that they are infected. That’s why it’s important for everyone to wear masks in public settings and practice social distancing (staying at least 6 feet away from other people).
- While masks are strongly encouraged to reduce the spread of COVID-19, CDC recognizes there are specific instances when wearing a mask may not be feasible. In these instances, adaptations and alternatives should be considered whenever possible (see below for examples).
People who know or think they might have COVID-19
- If you are sick with COVID-19 or think you might have COVID-19, do not visit public areas. Stay home except to get medical care. As much as possible stay in a specific room and away from other people and pets in your home. If you need to be around other people or animals, wear a mask (including in your home).
- The mask helps prevent a person who is sick from spreading the virus to others. It helps keep respiratory droplets contained and from reaching other people.
Caregivers of people with COVID-19
- Those caring for someone who is sick with COVID-19 at home or in a non-healthcare setting may also wear a mask. However, the protective effects—how well the mask protects healthy people from breathing in the virus—are unknown. To prevent getting sick, caregivers should also continue to practice everyday preventive actions: avoid close contact as much as possible, clean hands often; avoid touching your eyes, nose, and mouth with unwashed hands; and frequently clean and disinfect surfaces.
Who Should Not Wear a Mask
Masks should not be worn by:
- Children younger than 2 years old
- Anyone who has trouble breathing
- Anyone who is unconscious, incapacitated, or otherwise unable to remove the mask without assistance
Feasibility and Adaptations
CDC recognizes that wearing masks may not be possible in every situation or for some people. In some situations, wearing a mask may exacerbate a physical or mental health condition, lead to a medical emergency, or introduce significant safety concerns. Adaptations and alternatives should be considered whenever possible to increase the feasibility of wearing a mask or to reduce the risk of COVID-19 spreading if it is not possible to wear one.
For example,
- People who are deaf or hard of hearing—or those who care for or interact with a person who is hearing impaired—may be unable to wear masks if they rely on lipreading to communicate. In this situation, consider using a clear mask. If a clear mask isn’t available, consider whether you can use written communication, use closed captioning, or decrease background noise to make communication possible while wearing a mask that blocks your lips.
- Some people, such as people with intellectual and developmental disabilities, mental health conditions or other sensory sensitivities, may have challenges wearing a mask. They should consult with their healthcare provider for advice about wearing masks.
- Younger children (e.g., preschool or early elementary aged) may be unable to wear a mask properly, particularly for an extended period of time. Wearing of masks may be prioritized at times when it is difficult to maintain a distance of 6 feet from others (e.g., during carpool drop off or pick up, or when standing in line at school). Ensuring proper mask size and fit and providing children with frequent reminders and education on the importance and proper wear of masks may help address these issues.
- People should not wear masks while engaged in activities that may cause the mask to become wet, like when swimming at the beach or pool. A wet mask may make it difficult to breathe. For activities like swimming, it is particularly important to maintain physical distance from others when in the water.
- People who are engaged in high intensity activities, like running, may not be able to wear a mask if it causes difficulty breathing. If unable to wear a mask, consider conducting the activity in a location with greater ventilation and air exchange (for instance, outdoors versus indoors) and where it is possible to maintain physical distance from others.
- People who work in a setting where masks may increase the risk of heat-related illness or cause safety concerns due to introduction of a hazard (for instance, straps getting caught in machinery) may consult with an occupational safety and health professional to determine the appropriate mask for their setting. Outdoor workers may prioritize use of masks when in close contact with other people, like during group travel or shift meetings, and remove masks when social distancing is possible. Find more information here and below.
Masks are a critical preventive measure and are most essential in times when social distancing is difficult. If masks cannot be used, make sure to take other measures to reduce the risk of COVID-19 spread, including social distancing, frequent hand washing, and cleaning and disinfecting frequently touched surfaces.
Masks with Exhalation Valves or Vents
The purpose of masks is to keep respiratory droplets from reaching others to aid with source control. However, masks with one-way valves or vents allow air to be exhaled through a hole in the material, which can result in expelled respiratory droplets that can reach others. This type of mask does not prevent the person wearing the mask from transmitting COVID-19 to others. Therefore, CDC does not recommend using masks for source control if they have an exhalation valve or vent.
Face Shields
- A face shield is primarily used for eye protection for the person wearing it. At this time, it is not known what level of protection a face shield provides to people nearby from the spray of respiratory droplets from the wearer. There is currently not enough evidence to support the effectiveness of face shields for source control. Therefore, CDC does not currently recommend use of face shields as a substitute for masks.
- However, wearing a mask may not be feasible in every situation for some people for example, people who are deaf or hard of hearing—or those who care for or interact with a person who is hearing impaired. Here are some considerations for individuals who must wear a face shield instead of a mask:
- Although evidence on face shields is limited, the available data suggest that the following face shields may provide better source control than others:
- Face shields that wrap around the sides of the wearer’s face and extend below the chin.
- Hooded face shields.
- Face shield wearers should wash their hands before and after removing the face shield and avoid touching their eyes, nose and mouth when removing it.
- Disposable face shields should only be worn for a single use and disposed of according to manufacturer instructions.
- Reusable face shields should be cleaned and disinfected after each use according to manufacturer instructions or by following CDC face shield cleaning instructions .
- Plastic face shields for newborns and infants are NOT recommended.
- Although evidence on face shields is limited, the available data suggest that the following face shields may provide better source control than others:
Surgical Masks
Masks are not surgical masks or respirators. Currently, those are critical supplies that should continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance. Masks also are not appropriate substitutes for them in workplaces where surgical masks or respirators are recommended or required and available.
Recent Studies:
- Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. The New England journal of medicine. 2020;382(10):970-971. PMID: 32003551external icon
- Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral Load in Upper Respiratory Specimens of Infected Patients. The New England journal of medicine. 2020;382(12):1177-1179. PMID: 32074444external icon
- Pan X, Chen D, Xia Y, et al. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet Infectious diseases. 2020. PMID: 32087116external icon
- Bai Y, Yao L, Wei T, et al. Presumed Asymptomatic Carrier Transmission of COVID-19. Jama. 2020. PMID: 32083643external icon
- Kimball A HK, Arons M, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility — King County, Washington, March 2020. MMWR Morbidity and mortality weekly report. 2020; ePub: 27 March 2020. PMID: 32240128external icon
- Wei WE LZ, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic Transmission of SARS-CoV-2 — Singapore, January 23–March 16, 2020. MMWR Morbidity and Mortality Weekly Report. 2020;ePub: 1 April 2020. PMID: 32271722external icon
- Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science (New York, NY). 2020. PMID: 32179701external icon
- Furukawa NW, Brooks JT, Sobel J. Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic [published online ahead of print, 2020 May 4]. Emerg Infect Dis. 2020;26(7):10.3201/eid2607.201595. Link
- Oran DP, Topol Prevalence of Asymptomatic SARS-CoV-2 Infection: A Narrative Review [published online ahead of print, 2020 Jun 3]. Ann Intern Med. 2020;M20-3012. PMID: 32491919external icon
- National Academies of Sciences, Engineering, and Medicine. 2020. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020). Washington, DC: The National Academies Press. https://doi.org/10.17226/25769external icon.
- Schwartz KL, Murti M, Finkelstein M, et al. Lack of COVID-19 transmission on an international flight. CMAJ. 2020;192(15):E410. PMID: 32392504external icon
- Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering. N Engl J Med. 2020 Apr 15. doi:10.1056/NEJMc2007800. PMID: 32294341external icon
- Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A. Testing the efficacy of homemade masks: would they protect in an influenza pandemic? Disaster Med Public Health Prep. 2013;7(4):413-8. PMID: 24229526external icon
- Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S. Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks. ACS Nano. 2020 Apr 24. PMID: 32329337external icon
- Aydin O, Emon B, Saif MTA. Performance of fabrics for home-made masks against spread of respiratory infection through droplets: a quantitative mechanistic study. medRxiv preprint doi: https://doi.org/10.1101/2020.04.19.20071779, posted April 24, 2020.
- Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020. PMID: 32232986external icon
- Leung, N.H.L., Chu, D.K.W., Shiu, E.Y.C. et al.Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020. PMID: 32371934external icon
- Johnson DF, Druce JD, Birch C, Grayson ML. A quantitative assessment of the efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza infection. Clin Infect Dis. 2009 Jul 15;49(2):275-7. PMID: 19522650external icon
- Green CF, Davidson CS, Panlilio AL, et al. Effectiveness of selected surgical masks in arresting vegetative cells and endospores when worn by simulated contagious patients. Infect Control Hosp Epidemiol. 2012;33(5):487‐494. PMID: 22476275external icon